
Is It Time to Consider Surgery for Your Bunion?
Bunions can range in severity, from a small deformity with minor discomfort to an extreme and noticeable deformity that causes significant pain and physical limitations.
Bunions occur when the bones of your big toe rotates out of alignment and turn it inward. This causes the head of the metatarsal to jut outward, and creates that characteristic bunion bump on the side of the foot.
The size of your bunion increases along with the malalignment, which can produce an increase in symptoms and the need to truly address the problem. Left uncorrected, bunions can lead to other, more serious, foot problems.
Many people with mild bunions live pain-free and don’t require surgical treatment, but those with more severe bunions may require it.
People put off getting surgery for many reasons ranging from concerns about being out of work for an extended period, to worry about the pain it might cause.
If you’re experiencing any of the following due to your bunion, it may be time to consider discussing surgery with a physician:
• Pain when you’re on your feet for long periods
• Giving up your favorite shoes, either because of pain or because of the way the bunion makes your foot look
• Changing your lifestyle to accommodate your bunion
Sammy Gets Fed Up With Bunion Pain
Like many other people with bunions, Arthrex Minimally Invasive Bunionectomy patient Sammy tried conservative, nonsurgical treatments for the painful bunion on her big toe and the bunionette located on her small toe. She used silicone gel bunion “correctors” that wrapped around her toe and opted for different styles of shoes, or went barefoot altogether when she could to avoid the pain associated with the sneakers she often wore.
”A lot of the home remedies, I just didn’t have great success with,” Sammy says.
There are numerous nonsurgical options for treating your bunion, from special shoes to splints and spacers. These short-term bunion pain remedies may not permanently straighten your toe, keep your bunion from getting bigger, or prevent your bunion pain from getting worse.
For Sammy, the decision to consider surgery didn’t take very long.
Sammy’s life is filled with physical activity, including daily CrossFit® workouts and long walks with her rescue dog, Nova. Her job as a coach also requires her to be very active. Bunion pain that limited her activities wasn’t something she wanted to live with.
“Being on my feet for long periods of time was dreadful, honestly. It was really painful,” she says. “The aching would just progress throughout the day, and if I was wearing the wrong pair of shoes, it ruined my entire day.”
After briefly trying those unsuccessful home remedies, she spoke with a doctor in her area trained in the Arthrex Minimally Invasive Bunionectomy procedure about her surgical options. Although she had been reluctant in the past to undergo surgery for a different injury, her bunion pain was too constant to ignore.
What Does “Minimally Invasive” Really Mean?
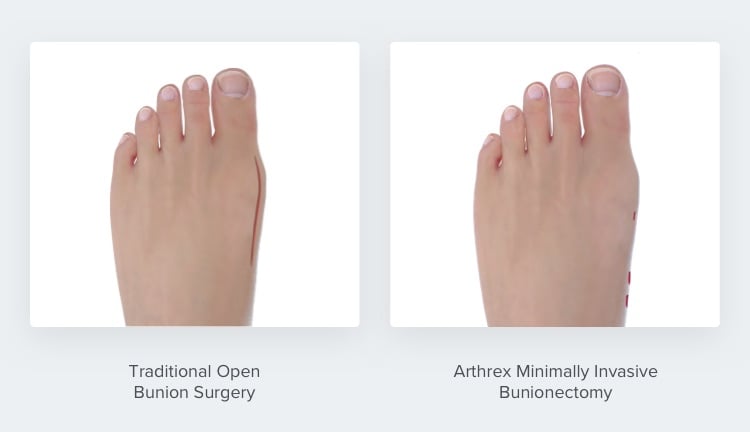
Traditional “open” bunion surgery procedures are considered invasive because they require large incisions, which may result in larger scars.
Baltimore, MD, foot and ankle surgeon Noman A. Siddiqui, DPM* once performed traditional open procedures but now performs the Arthrex Minimally Invasive Bunionectomy with good patient results, he says.
There are also procedures called minimally invasive that are not truly minimally invasive, says Christopher W. Hodgkins, MD*, a Miami, FL, orthopedic surgeon who performs the Arthrex Minimally Invasive Bunionectomy procedure.
“They require proper, formal, traditional incisions that might be smaller than prior, traditional procedures, but they still are not minimally invasive. They still require significant surgical dissection, which really makes them not a minimally invasive surgery.”
In the Arthrex Minimally Invasive Bunionectomy, incisions are tiny “pinholes.” Through those incisions, the surgeon realigns the toe bone and checks the alignment on x-ray. Once it’s in the right place, the surgeon fixes the bone with screws, Dr. Siddiqui explains.
“We never invade the joint. We don’t have to ‘shave’ the bump,” which can help prevent stiffness, Dr. Siddiqui says.
Why Should I Consider the Arthrex Bunionectomy to Treat My Bunion?
In her research about bunions and bunion surgery, Sammy came across numerous options for bunion treatment. She also spoke to an acquaintance who underwent traditional open bunion surgery, who warned her about the long recovery time she experienced.
“I think that was probably my first question to my doctor: How long am I going to be out?” Sammy says. Her surgeon recommended the Arthrex Minimally Invasive Bunionectomy because of its faster recovery time compared to other procedures.¹𝄒²
Dr. Hodgkins also recommends the Arthrex Bunionectomy to his patients for the faster recovery, in addition to other benefits.
“Those small incisions lead to almost no surgical scars and far less pain, which leads to a faster restoration of comfort, motion, and strength² after surgery,” he says.
Sammy is pleased her doctor recommended the Arthrex Minimally Invasive Bunionectomy for all those reasons.
“My doctor explained that the Arthrex Minimally Invasive Bunionectomy was going to correct my bunion deformity, also make my foot look better cosmetically, and I wouldn’t have these huge scars. I’d have better recovery time, less pain due to the minimally invasive procedure, and those are exactly my results.”
Sammy is a real patient who was compensated for the time she took to share her personal experience with the Arthrex Minimally Invasive Bunionectomy.
*Dr. Noman A. Siddiqui and Dr. Christopher W. Hodgkins are paid consultants of Arthrex, Inc.
References
- Lee M, Walsh J., Smith MM, Ling J, Wines A, Lam P. Hallux valgus correction comparing percutaneous chevron/Akin (PECA) and open scarf/Akin osteotomies. Foot Ankle Int. 2017;38(8):838-846. doi:10.1177/1071100717704941
- Lai MC, Rikhraj IS, Woo YL, Yeo W, Ng YCS, Koo K. Clinical and radiological outcomes comparing percutaneous chevron-Akin osteotomies vs open scarf-Akin osteotomies for hallux valgus. Foot Ankle Int. 2018;39(3):311-317. doi:10.1177/1071100717745282



